Hospital & Health Systems Revenue Cycle Management
Automated and data-driven revenue cycle management solutions to streamline operations, enhance efficiency, and boost reimbursement levels.
Redefining your Revenue Cycle for Financial Success
Helping health systems achieve a remarkable 99.7% first-pass acceptance rate with payers, Quadax goes beyond just being a medical claims clearinghouse. A four-time recipient of the Best in KLAS award for Claims Management, our innovative Revenue Cycle Management solutions are powered by automation and analytics to streamline medical billing processes for improved efficiency, enhanced visibility and control over financial operations to maximize reimbursement. Our EDI solutions leverage advanced technology to optimize areas within your revenue cycle, accelerating claims processing and reimbursement. This allows you to prioritize delivering top-notch patient care without sacrificing your financial goals.
Advanced Claim Status
Advanced Claim Status (ACS) seamlessly incorporates a more detailed and comprehensive claim status update into your workflow, enhancing efficiency for your team and facilitating increased automation.
Contract Management
Contract Management analyzes contract variations and compares expected reimbursement to allowed amounts, enabling organizations to identify underpayments, denials, and shortfalls, and take action to prevent revenue leakage.
Eligibility
Insurance Eligibility confirms a patient’s insurance coverage and benefits, delivering details on copays, coinsurance, and deductibles in real-time to prevent claim rejections, payment delays, or revenue loss.
Verify Medicare and Medicaid Eligibility
Utilize HETS (the HIPAA Eligibility Transaction System) to confirm eligibility and verify Medicare and Medicaid coverage using Integrated Coverage Validation (ICV) for efficient claims processing, enhanced compliance, and accelerated reimbursements.

Xpeditor
Integrated Workflow Automation
Quadax’s Xpeditor software streamlines workflow by directing claims efficiently to designated billers based on your criteria, ensuring a precise audit trail, and eliminating reliance on external communication channels. By integrating workflow automation between Claims Management and EHRs or billing applications, processes are optimized to enhance clean claim rates, reduce overhead costs, and empower you with the tools needed to swiftly and effectively recover expected reimbursements.

XpressBiller
Auto Fix and Scrub Claims with Custom Rules & Edits
To improve clean-claim rates, start with proactive measures. With XpressBiller, Quadax’s cutting-edge rules and editing system, automatically pinpoint, address, and reduce errors in real-time before submitting claims to the payer. By tackling the root causes that impede claims and cut into profits, you can take charge of your revenue cycle and satisfy even the most challenging payers without the need for IT involvement and at no extra cost.
Eliminate Paper EOB & Correspondence Bottlenecks
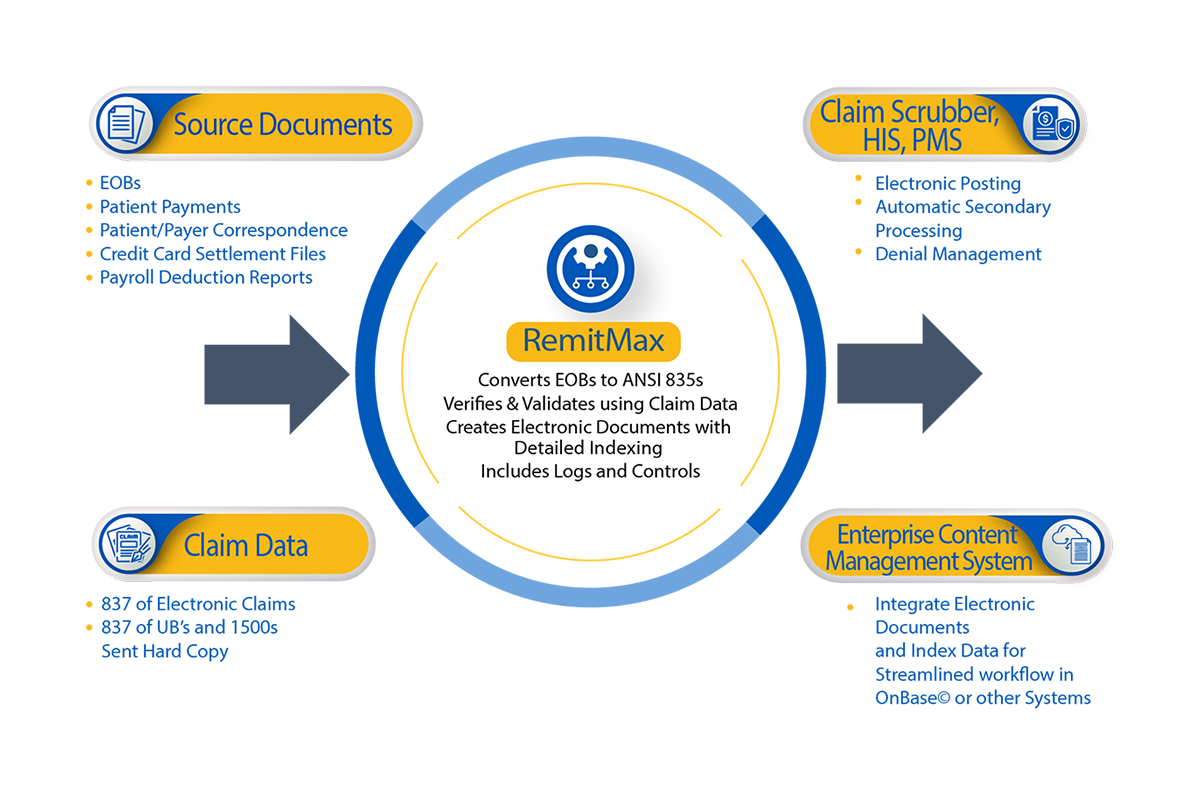
RemitMax
Streamline your billing office workflow and saves those hard-earned dollars by eliminating paper with RemitMax by Quadax.
Adding RemitMax to your remittance management strategy allows you to get control of all your remittance and correspondence documents—even patient payments—that you or your lockbox now receive on paper. And, the 835s created by RemitMax are subject to the same automation that’s afforded within the Claims Management and Denial Management solutions, such as automated COB claims, denial management workflow and robust data analytics allowing for a more accurate picture of the entire revenue cycle.

Intelligence By Quadax™
Revenue Cycle Analytics & Reporting
Intelligence by Quadax™ leverages cutting-edge tools and cloud services to continuously gather and analyze your intricate revenue cycle data from various systems, consolidating it into a single, reliable source. Uncover key drivers, explore cause-and-effect relationships, unearth opportunities, and track performance against internal targets and industry standards. Effortlessly export reports or showcase real-time data and analytics visually for executive presentations or comprehensive reports.
Avoid guesswork – understand payer requirements by analyzing payer data trends, addressing revenue losses and time constraints, and identifying opportunities for improved efficiency. Stay informed about current and future strategies to empower your finance and billing teams to collaborate effectively with your commercial sales and payer relations group.
Why Our Clients Choose Us
Samaritan Medical Center
“Quadax stood out because their data goes beyond individual pieces of information and offers a comprehensive view. It allows us to identify areas for improvement and chart a path to increase our reimbursement.”
— Chris Hochgraf, Director of Revenue Cycle
Claims & Reimbursement Support Services
Rely on the Experts
Quadax revenue cycle experts offer regular on-site visits to help with event management and resolution, ongoing training, customized reporting solutions, industry best practices, and overall issue resolution. With Quadax, you’ll experience a seamless integration of advanced technology and dependable, personalized support.