PAMA Reporting for Labs
The Protecting Access to Medicare Act of 2014 (PAMA) revised the payment methodology for clinical diagnostic laboratory tests paid under the Medicare Clinical Laboratory Fee Schedule (CLFS). In accordance with PAMA, CMS will determine the payment rates for the clinical laboratory fee schedule in 2025 based on the rates reported by applicable laboratories from private payers.
Meet Compliance Requirements with Quadax
CMS Further Delays PAMA
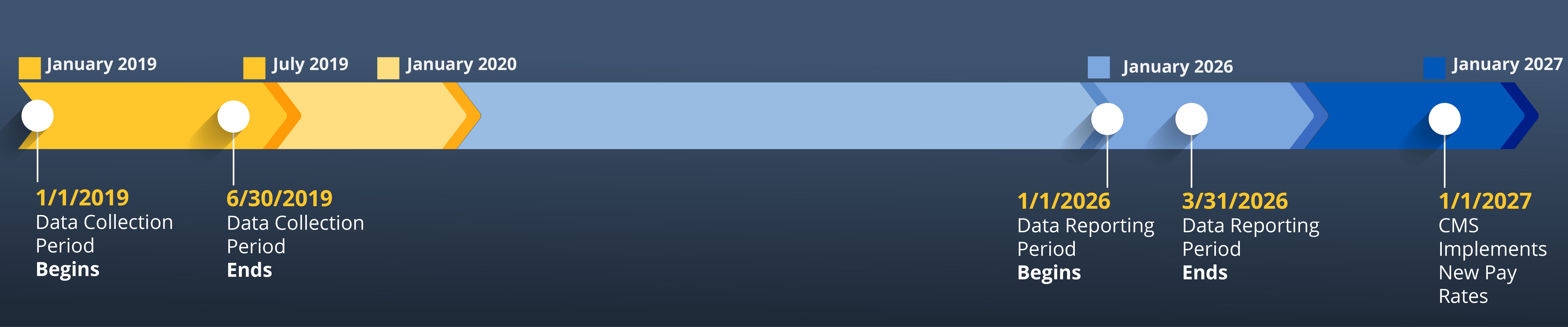
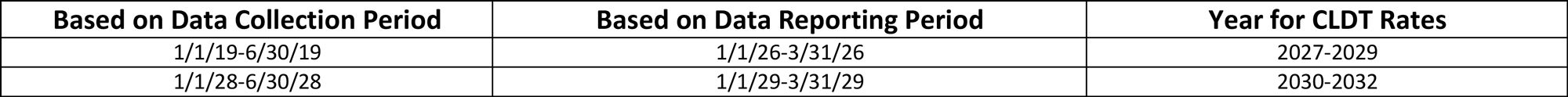
In September 2024, the Continuing Appropriations and Extensions Act of 2025 delayed the PAMA data reporting period from 2024 to 2026. Applicable laboratories were given an additional year to report final payment data collected during the first six months of 2019.