AI-powered solutions can improve healthcare reimbursement rates through intelligent error detection and process optimization.
![]()
Stay informed on the latest industry news, best practices, and trends in revenue cycle management for hospitals and physician groups.
“Quadax takes a partner approach. Coming from other vendors, I’ve found that Quadax’s solutions are more user-friendly. The integration of their Predictive Intelligence tool surpassed my expectations by effectively demonstrating its ability to exceed our reimbursement goals.”
– Stacy Walls, Medical Billing Manager at Crisp Regional Hospital
CASE STUDY
CLIENT: Crisp Regional Hospital (Cordele, Georgia)
CLIENT INFORMATION: Crisp Regional Health Services oversees the award-winning, high-tech Crisp Regional Hospital with a level 3 trauma center. Its comprehensive network of health and social service facilities includes a home health program, 143-bed nursing home, retirement home, hospice and home care program, dialysis facility, and rural health clinics in bordering areas. More than 50 physicians practice within Crisp Regional Hospital, providing hospital and outpatient care in family medicine, obstetrics/gynecology, emergency medicine, and 20-plus other specialties and subspecialties.
OPPORTUNITY: As a longstanding client of Quadax, Crisp Regional Hospital aimed to explore opportunities for avoiding denials within their revenue cycle. Having achieved significant success with Quadax’s existing solutions, Crisp expressed interest in further reducing their denial rates by targeting specific error categories. Quadax partnered with Crisp to implement Predictive Intelligence by Quadax (PIQ), with the goal of having the ability to predict coding errors and non-covered errors before claim submission to payers, thereby reducing manual workload and delivering substantial ROI.
Predictive Intelligence by Quadax (PIQ) is a powerful predictive model, built with machine learning technology, to transform denial management into denial avoidance, helping you to get paid as quickly as possible. By combining claims and remittance processing with machine learning tools, Quadax built the industry’s most powerful predictive model for revenue cycle optimization.
SOLUTION: While exploring Crisp’s denial avoidance opportunities, Quadax discovered the largest opportunity existed in their coding and non-covered error codes. While building the PIQ model designed specifically to the client, Quadax discovered a trend within their data and established an XpressBiller rule to flag these claims within their Denial Prediction workflow. By setting this new rule, Crisp was able to adjust their previously denied claims and correct them, resulting in a recovery of more than $93,000 which had previously been written off.
By leveraging automated rules within PIQ, Crisp’s claims were halted and predicted edits were remedied before the claim was released, resulting in a reduction in manual labor from encounter to claim release due to limited touches by staff.
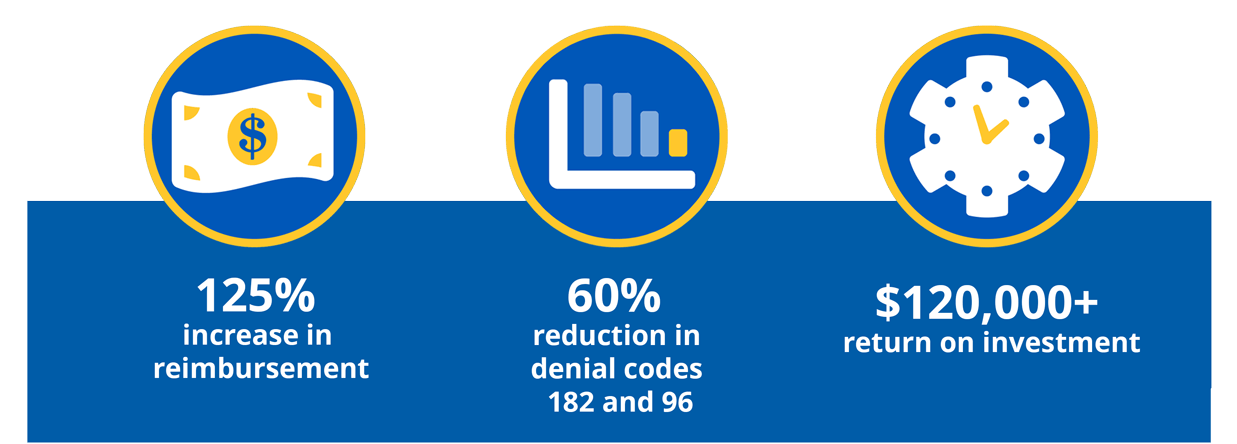
ACHIEVING SUCCESS: Predictive Intelligence by Quadax transforms denials into recovered revenue for Crisp Regional Hospital
Utilizing PIQ as an invaluable training resource, Crisp was able to use the predictions from PIQ to aide in remediating claims, allowing their new users to see cause and effect in real time.
By integrating PIQ within Quadax’s claims management solution, Crisp Regional Hospital is able to reap the benefits of the most powerful predictive model for revenue cycle optimization, providing them with the ability to predict errors before they are released. This integration has “proven there is ROI.”
“Implementing PIQ into our existing workflow has exceeded our expectations and recovered money.”
-Marilee Bruns, Director of Patient Financial Services, Crisp Regional Hospital