The financial impact of PAMA to your laboratory depends largely on the type of testing you perform. With the recent publication of the 2018 Medicare CLFS reimbursement rates, it is clear that high-volume clinical laboratory testing is facing substantial downward pricing pressure while much of the advanced molecular diagnostics and genomic testing market reimbursement is neutral to positive. Because of this, it is not surprising that two influential industry groups, the American Clinical Lab Association (ACLA) and Coalition for 21st Century Medicine (C21), have issued opposing statements about the implementation of PAMA. Notwithstanding a successful last-minute legal challenge by those opposing PAMA, the industry must prepare for the likelihood and reality of an implementation on January 1st, 2018. If you haven’t done so already, knowing how PAMA will impact your lab’s revenue is a critical next step in this preparation.
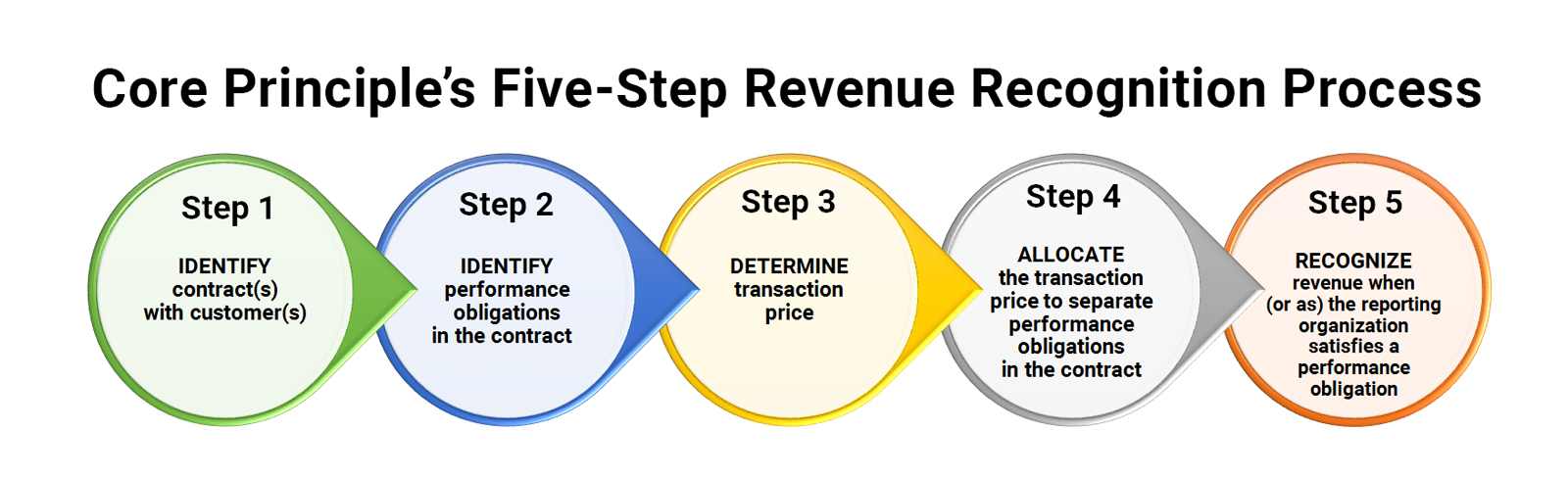
The Protecting Access to Medicare Act of 2014 (PAMA) revised the payment methodology for clinical diagnostic laboratory tests paid under the Medicare Clinical Laboratory Fee Schedule (CLFS). Final Payment rates released November 17, 2017 will be implemented effective January 1, 2018. Studying Medicare’s new market-based payment system for laboratory services, there are areas of opportunity. Preliminary analysis indicates that molecular and genetic diagnostic testing services may benefit from the new rates. Other clinical testing services may experience a decrease in rates, in which case it becomes very important to understand which claim populations are impacted. may need to apply more complex financial models. All laboratories should also consider PAMA’s secondary impact on commercial payers (both contracted and non-contracted) who derive their allowed amounts from the prevailing Medicare CLFS. Trying to determine the exact impact PAMA will have on your lab can be its own challenge.
Quadax has developed a proprietary modeling tool that is helping our laboratory clients plan and prepare for PAMA’s initial and on-going impact. By using this tool to identify and quantify areas of greatest challenge and opportunity, our client service teams provide the data to help drive our customer’s decision-making process. To deliver the best results, we collaborate with our clients bringing together our joint expertise in the analysis and interpretation of the data, reporting requirements, and clinical aspects of the tests. If you are interested in learning more about our proprietary PAMA modeling tool and how we can use it to benefit your lab, please contact us. We are here to help.
As your lab considers future opportunities—from enhanced operating efficiencies to test menu diversification—an optimized revenue cycle management solution is key. One that solves for both tactics and strategy so that reimbursement efforts maximize revenue in the new world of PAMA-driven pricing.